Self-directed support, with careful planning, could be a great help to the well-being of people with fluctuating mental health.
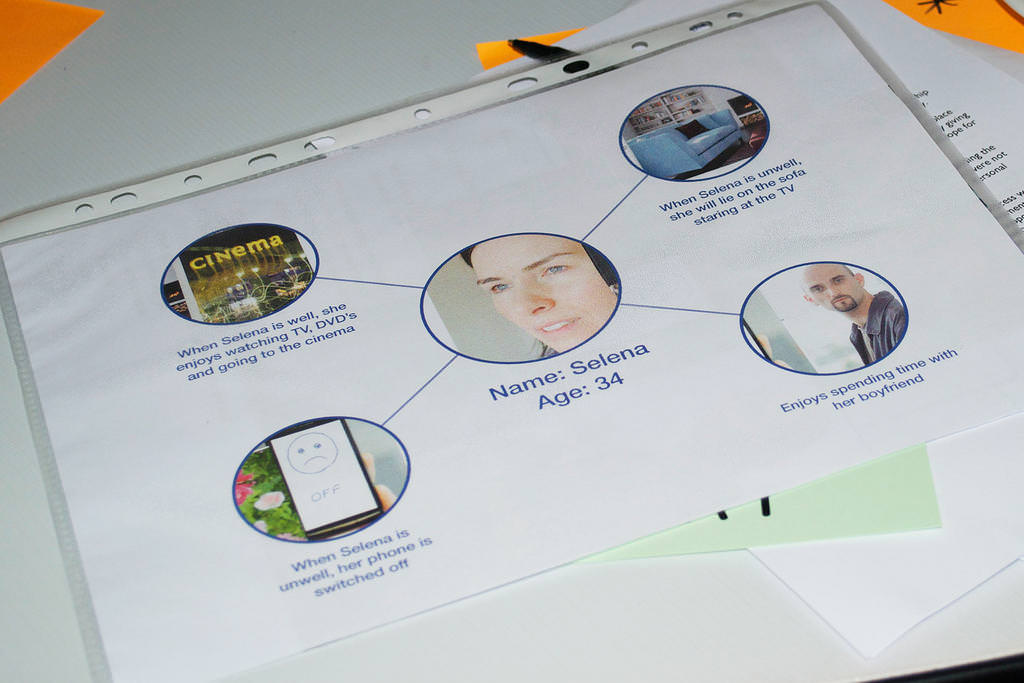
The planning and form filling parts of the assessment should always be done when the person concerned is in a “well and positive mode”. Who does the assessment with the person concerned is also very important. It must always be done by a worker with mental health training, preferably by someone already known and trusted. A worker not familiar with the mental health history of the person might think that in a “well period” the person does not seem to be in need of extra help. A worker known to the person knows the need to keep them on a stable pathway and also the psychological behaviour of the person when they are unwell. Discussions with the person when they are well enables the best plans for their continual well-being and addresses making a plan for when they are unwell.
As it is the nature of some mental health illnesses that the person does not always know when they have crossed over the line from being well to being unwell, this would be especially important if the person was in charge of their own budget. A third party may need to be involved to judge the state of mental health enabling the person to make their own decisions or at what point a third designated party take over such decisions.
If these plans are made with a lot of forethought it could be very beneficial to the client. I feel it needs three main points of planning:
- Planning for Wellness – and attaining achievable outcomes for the person in times of wellnesss, for example, social activities, group meetings, equipment for the enablement of hobbies (thus helping people to use their time in a productive way). People can expand their talents in crafts, arts etc. that could be focussed towards greater fulfilment with help with basic equipment; courses to enable learning – the choices are endless.
- Planning for unwellness – ensuring that the doors that have been opened for the above activities are not closed, and that people know that changes can be made to enable them to get more support, either in day centres, visits within their own homes or in other places that they feel is a safe environment. It is at these times that a third party is needed that the person trusts to either help them or make direct decisions for them, having only their well-being in mind.
- Re-introduction into wellness – and to the activities and plans originally put in place to help continuous well-being. This should be done at an agreed pace of introduction that the person is comfortable with.
Self-directed support I feel will be a perfect pathway for a big percentage of people with mental health problems, enabling them to take charge of their lives in a positive way and at the same time having the safety nets in place at times when they are unable to cope with day to day living with the help of their mental health team.
